Entities across the supply chain today are engaged in learning about how RFID will impact the way business will be conducted in the future. Retailers are pushing for adoption of RFID and at the same time manufacturers and logistics providers are trying to find out how to, minimally, comply with industry mandates.
The healthcare industry is one of the most regulated industries in the world. In almost every link of the supply chain there are reports to file with government, insurance carriers, manufacturers and quasi government associations concerning each medical device, instrument and supply. These filed reports are for patient and product safety and for reimbursement for services and products provided. In an industry where patient safety comes first, the lack of profitability in many healthcare providers has been reluctantly tolerated. Radio Frequency Identification (RFID) can improve patient safety and service as it seamlessly addresses the profitability through increased labor efficiency and inventory reduction and by automating healthcare providers main revenue-reporting component—charge capturing.
Some healthcare providers are piloting RFID in areas pertaining to patient safety and the tracking of expensive medical devices to increase their availability (asset visibility). These RFID projects have probably saved some lives. However, the true financial value in terms of returns on investment cannot be calculated on projects this small in scope. For realizing the full potential financial value of RFID, it is important to model and measure the returns in terms of asset utilization and cost. Therefore, the model we present defines the true value of one medical device or instrument and that item’s ROI, once RFID is implemented throughout a healthcare facility.
The following questions frame organizations’ expectations concerning the adoption of RFID technology:
• Given a mandate to deploy RFID technology, how will that affect the way we do business with our trading partners?
• Are there interim steps that will comply with the mandates and still yield a return on my investment?
• What is the best and most cost-effective way for us to integrate RFID in our operation?
• What are the expected returns on my investment?
In this paper, we hypothesize a unique approach that is best fitted for the healthcare market. We believe our approach can be applied to other industries. We will show how RFID can be cost-effectively implemented in the healthcare industry. This implementation will lower inventory costs, increase asset visibility and maximize labor productivity—resulting in higher profitability.
|
Bradley H. Sokol has started three emerging technology companies in a variety of industries. In 1999, he launched Electronic Directory Corp., an interactive, public-access, touch screen mapping directory for hospitals, tourism and commercial building developments. He has consulted in a variety of fields including healthcare coding for medical devices. He can be contacted by sending e-mail to [email protected]. Sapan Shah is a project leader for Patni Computer Systems, an India-based systems integrator. Patni’s dedicated RFID practice offers a complete range of RFID services as part of its enterprise application solutions. Sapan is actively involved with the developments of RFID within and outside Patni and regularly contributes to the industry forums. He can be contacted by sending e-mail to [email protected]. |
The Approach
We are writing this paper as independents due the unique position we are taking in solving many issues confronting a total RFID “end-to-end” healthcare supply chain integration. The ideas we present are solely ours and should not be associated with their respective organizations. The paper postulates are supported by extensive field research, where we have contacted globally over 200 individuals. Previous research has never been publicly offered concerning several proofs of our postulates. Our research and field studies enable us to extrapolate our cost justification assumptions. Everything we believe appears to be borne out by these observations and research. Our field research has found these figures are well within the parameters of acceptability.
Each section of this article frames the problem and provides a solution. Moreover, we suggest several viable interim solutions that can yield similar results. Finally, we project a different future supply chain model technically, operationally and financially.
As a different marketing approach to this paper, our “reviewers” agreed to view only their own section. The entire paper has never been exposed to any one entity. We have more than 30 well-established and globally recognized companies, organizations, individuals and associated cross-industry corroborators who have shared their knowledge regarding their applicable sections. These “reviewers” are only responsible for providing information, not the totality of the papers’ content or solutions.
Introduction
Many entities in the healthcare industry are implementing RFID pilot programs. The approach of their implementation is to evaluate only a group of valuable items of each component in the supply chain separately. We propose an approach that can assist in the building of an automated supply chain in an efficacious manner.
We believe that In order to obtain true economies of scale in RFID, one needs to also tag objects that have a minimal cost value ($95 to $5,000). The majority of an operation’s inefficiencies are found at a micro level (one wheel chair: $500). Tagging items at this value level will help improve the actual individual caregiver’s efficiency, regulatory compliance, organizational confidence and patient safety. The current projects don’t address the overall outcome due to their limited scope and concentration on only high-valued assets.
The micro modular approach is timely for the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) accredited healthcare provider due to a new JCAHO requirement for maintaining life support equipment. The “Shared Visions-New Pathways” initiative requires, in order to remain an accredited healthcare facility, they must demonstrate that life support equipment receives a high priority in their equipment maintenance programs. This regulatory initiative will drive these institutions to consider RFID as a means of easing the regulatory compliance, reporting and audits that will be strictly enforced by July 1, 2005. As regulatory compliance drives many industries, we believe that the healthcare provider supply chain link will be one of the next major healthcare industry segments to look at RFID as a possible solution.
The ultimate goal of RFID is to build a completely automated supply chain. However, there are issues preventing a fully integrated healthcare supply chain solution. Some of these issues are generic in any RFID project: Industry business environment, communication; data transfer, storage and verification, etc., all tend to make total supply chain integration a distant goal.
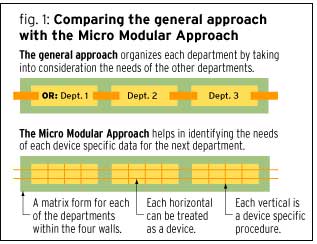
As shown in Figure 1, the currently accepted approach (the “general approach”) is to pilot an RFID project in one department that comprises only that department’s valuable assets above $3,000. Usually the pilot project goals are for increased patient safety and to track high-value shrinkage. We suggest an approach (the “micro-modular approach”) at the level of the medical object—the micro level. We assume the medical object to have it’s own four walls; just as any department or facility has four walls.
Within the healthcare industry, at the healthcare provider level, there are unique lifesaving requirements that dictate RFID implementation drivers that differ from those used within other industries. The micro-modular approach in Figure 1 divides each department into a matrix for a better visibility and higher returns. For instance, saving a life by a procedure, task, event (represented by the lower vertical boxes), performed by a scalpel, bedpan and medical object (represented by the lower horizontal boxes) conducted in the surgical department (Department 1), may take precedent over the other departments’ needs for the same medical object. Manufacturers call this process “just-in-time management.” The top row of horizontal boxes denotes other departments.
The viability of RFID in healthcare at a micro level can be proven as a closed-loop system, by viewing each procedure and department in the hospital, and how each single item is utilized. Once the micro-level systems are in place, one can then modularly build the entire RFID structure from the viewpoint of an individual product, with ROI achieved at each modular building block.
The key will be to develop cost and asset-reporting ends independently, while congruently monitoring the horizontal and vertical organizational issues. Additional considerations for RFID implementation are EPCglobal’s Electronic Product Code standards that are slowly evolving, new hardware technology and the convergence of the open systems and software development standards that should address future and current healthcare standards and regulations.
The Micro-Modular Approach
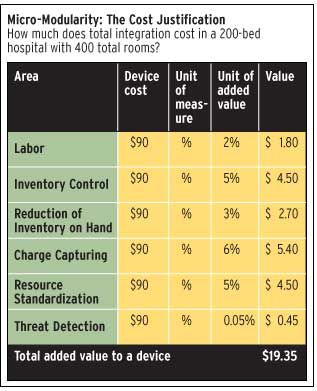
The healthcare industry needs to address declining profits due to increasing expenses, limited resources and declining reimbursements from public and private carriers. Given the present environment, the healthcare industry would undoubtedly invest in RFID if there were a solid financial case for improving profitability and operational efficiencies. However, a total end-to-end informational-systems and financial solution is currently not viable in the healthcare supply chain. Therefore, we suggest proving the supply chain’s viability within the “modular four walls”; first at the medical-object level then expanding the item’s value through the procedure, department and the facility.
An RFID item-level implementation uncovers the hidden true value of any object. The object’s true value will deliver the financial proof of RFID’s cost-effectiveness at the item level. An item’s true value is calculated on its list price and accounting for the many different repeated functions where it is used throughout the departments and in various procedures during its life expectancy. By properly calculating the single object’s true value—its life expectancy, usefulness across departments and in procedural events—the organization will be able to recover previously unrecorded efficiency gains of the object, thus resulting in the object’s true value.
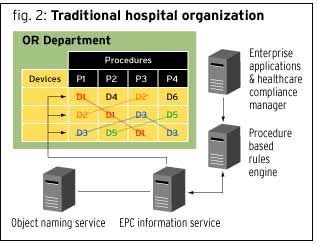
As shown in Figure 2, in a hospital organization environment, the vertical boxes represent the procedure, event or service such as surgery, X-rays, cleaning or distribution of supplies. Within each procedure represented by a vertical column (for example, P1), there are sets of medical objects associated with that procedure (in this example, D1, D2 and D3). These objects can be orthopedic devices, sutures, linens, catheters and diagnostic equipment. There are similar matrix configurations in each hospital department. The departments can be such things as an operating room, radiology or facilities management. Together, all the departments form the hospital’s horizontal hospital supply chain, as shown at the top of Figure 1.
In order to optimize the supply chain, each fundamental process in the healthcare industry—selection, requisition, order, manufacturing, transport, receive, inventory, distribute, point-of-use, pay provider, charge recipient, and reports—has its own information needs and requirements. Each process must be able to communicate to others in the supply chain.” The end goal of any approach taken by anyone in any vertical market will be to integrate and/or automate the entire supply chain.
The micro-modular approach, specifically, strives to resolve many of the existing issues in the life sciences industry. Given that when the approach is fully implemented in the organization, the ROI will increase throughout the supply chain of the hospital. The micro-modular approach for RFID promises to get the most out of your investment by maximizing your limited resources and properly employing them so that the Micro Modular process could eventually automate the entire supply chain.
The difference the Micro-Module Approach makes
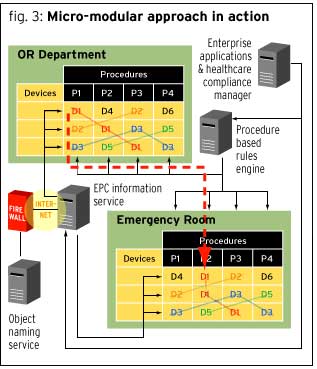
It is quite likely that one medical device is used in multiple procedures within the same department. Additionally, the same object may be used in a number of different procedures in different departments. In Figure 3 each separate horizontal block is an object, item or instrument (note D for device and 1 to signify the first device). The vertical row is a procedure with all the necessary items to complete that procedure (note P for procedure and 1 for the first procedure). In the OR Department, for example, procedure P1 uses devices D1, D2 and D3; in the Emergency Department, procedure P1 uses devices D4, D2 and D3.
By dividing each department into a matrix of horizontal boxes representing medical devices and vertical rows representing procedures, one can track the reusability (repetitive use) of one item/device through the organization’s multiple departments. This visual matrix shows how to maximize asset and operational planning of each tracked item, increasing the resulting in ROI through gained asset and operational efficiencies, thus yielding the items true utility (value). Figure 3 shows how device D1 can be used in the OR department in procedures P1, P2 and P3. The same device, D1, is used again in the Emergency Department in procedures P2 and P3.
The Micro-Modular approach divides each department into horizontals devices and verticals procedures, giving a clear picture for the needs (value) of every object relative to its usefulness to perform different tasks in a variety of procedures and within the scope of different departmental functions.
ATTACHMENTS
Previous research has never been publicly offered concerning several proofs to our postulates. We have done extensive research and some field interviews to extrapolate our cost justification assumptions. Everything what we believe appears to be borne out by these observations and research. Our field research has found these figures are well within the parameters of acceptability. This section explains the figures we used.
Labor estimate per device (national averages):
–Operating Rooms per Hospital: 8
–Number of procedures performed in a day for an operating room: 8
Asset visibility (time saved per day)
–Time searching for equipment, site verification before and after procedure, sequential stockings
–Number of operating rooms x number of procedures x average minutes saved= Average saved minutes a day.
–8 Operating Rooms x 8 Procedures x 9 average minutes a saved = 576 minutes
Workflow: Field studies claimed this was a soft cost
–Automation of “Chart count” and patient paper work.
–Faster set up and clean up of surgical room.
CFO’s suggested this was a soft cost because people are already doing that work. However this would add an additional 256 Minutes
Improving sequence: Checking for epired items/recycling of unused sterile supplies
–Number of operating rooms x number of procedure x average minutes saved31 = Average Minutes saved a day.
–8 OR x 8 Procedures x 4mins = 256 minutes
Labor fixed cost
–Average salary and benefits of one surgical team made up of 2 doctors and 3 nurses (not counted in labor amount are indirect support,
1 administrator, 1 housekeeping staff, 1 aid and 1 orderly) : $1,400,000, ÷ 10,400 hrs a year (5 people x 2,040hrs a year) / 60 minutes an hour = $2.25 a minute.
–Total timesaving = 832 minutes or 13.87 hours a day (2 persons), which is time for one additional OR procedure per day.
Total time savings a day x average earning per minute = total cost savings a day: 832 minutes x $2.25 a minute = $1872 a day savings
Cost per device in labor
–Daily savings divided by average number of items (36,000) in a hospital: $1,872 savings a day ÷ 36,000 items in a hospital = 5.2 cents per device a day.
–Total hard labor savings for a hospital per medical item is approximately 2 percent of labor cost in a hospital.
–Field research suggested that there is at least a 5 to 15 percent labor savings.
Assumptions
–35,000 reoccurring medical instrument turnover in inventory at 1.0 times a year.
–37,000 medical instruments or devices are on hand any given day
–If all the instruments of the hospital were allocated per bed, there would be 10 medical devices +58 instruments = 68 devices per bed.
–Hospital has a network.
RFID Equipment Required
–70,000 passive 13.56 MHz tags, 2,000 active (battery-powered) tags
–Active and passive readers, handhelds and mounted
–Antennas
–RFID middleware
Assumptions for Cost Justification
–10 medical devices average life = 6 years
–10 average number of devices per bed = 10 total devices needed a year per bed x 200 beds= 2,000 required per year
–58 hospital instruments allocated per bed x 300 percent stock on hand= 175 plus one inventory turn of an additional 175 x 200 beds= 70,000 per year. This number includes instruments in other departments.
–Patients room = 16.4 per bed
–OR 240 items x 8 rooms = 1,920 ÷ 200 beds = 9.6 per bed
–Remaining hospital 16 departments x 525 items per depart = 8,400 ÷ 200 beds= 42.0 per bed
–Physio, Bio lab, Ambulatory, Pediatric, Radiology, Cardiology
–Acute Care, Pharmacy, Pathology, Emergency, Oncology,
–Orthopedics, Medical Billing, Facilities Management, Information Systems,
–Patient Administration, Medical Laboratory
Total : 68 per bed
Costs Based on the following Assumptions
Tags
–Assumption: Labor costs = 50 cents a tag
–Tags cost, including labor
2,000 active tags at $12 each = $24,000
+ 35,000 passive tags at 75 cents = $26,250
Total = $50,250
Inventory turn: Annual cost of tag replacement, including labor.
75 cents x 35,000 tags= $26,250
Readers and Antennas
–Readers 300 passive readers at $600 each = $180,000
–Readers 200 active readers at $1,000 each= $200,000
–Antennas: each 1 reader can handle 4 antennas.
–800 antennas at $150 each = $120,000
RFID Physical installs
–Assumption: 10 people for one month at 150 hours each
–RFID Physical install (readers, antennas, wiring): 1,500 hours at $100 an hour = $150,000
Change in Process
–Assumption: $50 is average IS in-house hourly cost and 8 people at –125 hours a month for two months.
–Change in process: 2,000 man hours at $50 an hour = $100,000
System and Hardware Upgrade Cost
–Assumption: Middleware is $30,000; hardware, networking, LAN = $70,000.
–Medical financial, supply, materials management software = $400,000.
–System and hardware upgrade cost for tracking and OR software = $500,000
Training of Staff
–Assumption: $50 an hour x 2 (because a person being trained is while not doing his job while in class); 25 people at 16 hours each.
–Training staff: 400 hours at $100 per hour= $40,000
Total: $1,366,500
–Total cost of an RFID project per item = $1,366,500 ÷ 72,000 devices= total added cost of a device: $18.98
–Total Value of Each Device:$99.35
($90 original cost + $9.35 added value)
–RFID Cost per Device: $98.98
($1,366,500 divided by 72,000)
Difference: $0.37
Justification for the combination of readers and tags
Background information on physics provided by InfoWave Solutions, CEO, Rich McGillicuddy
Cost of Active Tags
One of the big issues with the active tags is the cost. Even at $12 each, the tags are very expensive. The price of these tags is on its way down, to below $10 in the near future. But even at $12 with (0.3 percent shrinkage of tags per day), the daily cost of the tag is $0.04 (estimated battery life of 7 years at a 2.5 chirp rate). If an IV Pump costs $25 per month to lease, the additional $1.50 to make sure that your utilization is high and shrinkage is low, seems like a smaller price to pay
Reader/Antenna Placement
Readers for Passive Tags
At points of consumption or execution, deploy simple tabletop readers that provide visual or audible indicators to let the personnel know that the items have been read. Install a separate set of readers at a chute or conveyor located at inventory areas for quick inventory check-in and department-to-department delivery, and at points of execution where the items needed for the procedure are bubble packed.
Readers for Active Tags
Active tags require readers in or around the ceiling and probably one every room for the coverage area. This area could be the whole hospital or specific floors or departments, depending on how detailed you want coverage. Realize that if you do not cover an entire hospital, once the asset is outside the range of the readers, it appears lost or gone. You would know where and when it left your sight but not much more than that. You can also setup alerts and alarms if items go outside of prescribed areas or go through exits.