All CEOs wish they had a crystal ball, so they could see the future and prepare for it rather than simply react to change. Unfortunately, there’s no way to know what the world will be like in, say, 20 years. But we believe radio frequency identification will be widely adopted by 2030 and will have a profound impact not just on the way companies do business, but on the way people shop, travel, learn and more.
Exactly how this growth will take place isn’t clear, but there are signs. Technology providers that promote the benefits of RFID and deliver solutions to solve specific business problems, providing a fast return on investment, will lead the way. At the same time, companies that use the technology—to track assets and inventory, streamline operations and business processes, or provide customer services—will create and leverage an RFID infrastructure to achieve even more benefits.
|
|
In the scenarios on the following pages, we imagine what the world will be like in 2030. Read them, then ask yourself where your company will be 20 years from today. Will you be powering or using the solutions that attract shoppers to retail stores, expedite product shipments, put the joy back in travel, enhance education, simplify chores and save lives? Or will you be playing catch-up?
* * *
She stopped suddenly in front of the nurse’s station as the words streamed from the emergency broadcast system: “Explosion at the Kildeer Chemical Factory. Hundreds hurt. Number of deaths not yet determined.” Dr. Linda Henley’s first thought was: Not again.
As an intern, Henley had treated wounded when the Bunding plant caught fire 20 years ago, and it hadn’t been pretty.
Her second thought: This time, we’re prepared.
As Henley neared the chemical factory, traffic slowed to a crawl as police tried to clear the way for emergency vehicles. She pulled her car off the road, parked in a strip mall and ran the last mile or so to the disaster site.
The scene appeared to be total chaos—people running in all directions, sirens wailing, debris everywhere you turned—yet emergency medical personnel had already begun to band and treat victims. They used triage wristbands to indicate patient priority level and store digital diagnostic codes for—and data about—drugs and other treatment administered at the scene.
Henley made her way to a man who’d been severely burned. She pulled out the handheld computer she used in the hospital to receive messages and record treatments, and waved it near the man’s wrist. The computer indicated the man had been unconscious when removed from the facility. He’d been given a painkiller and medication to stabilize his condition. Henley tapped on the handheld device, selected “Requires Urgent Hospitalization” and wrote that data to the man’s wristband. A few minutes later, paramedics came through the area, identified those ready to be taken to the hospital and moved out the man with the burns.
Henley’s handheld vibrated, then her cell phone. The Texas Office of Emergency Management was setting up a command and control center in a trailer just outside the chemical complex, and she was to report there immediately. “Expect more than 200 injured,” a text message said. “The chemical company’s tracking system has accounted for most employees and visitors, but indicated that some people were still inside Sector B.”
Henley had participated in many drills since the OEM set up the Integrated Response System to address problems with coordination during the Bunding fire, which slowed the response and probably cost lives. But this was the first time the governor had activated the system for a real emergency.
In the control center, a dozen computers were set up on a long table and the room was cluttered with mobile telecommunications equipment. Rick Peterson, head of the OEM, was looking at a screen that showed the location of every ambulance in the region and its status—was it carrying a patient, available to respond to the disaster, in transit already?
“Get that vehicle on Lefferts Street out of the way. Direct all incoming ambulances to convoy up,” Peterson said. “Keep the line moving.”
The response team also could see the status of all emergency and operating rooms in trauma centers and other hospitals across the city, as well as those in neighboring counties that participated in the program. The system indicated the available beds in those facilities, as well as an inventory of critical equipment and supplies, such as oxygen pumps, blood, morphine and antibiotics. As hospitals, in accordance with the state’s Disaster Response Plan, moved all non-life-threatening cases out of the ER and canceled non-emergency surgeries, their status flashed from red to green on the computers in the command center.
Henley and two other doctors sat in front of computers and began coordinating patient evacuations. Each time the icon of a victim whose wristband indicated he or she was critical was dragged onto the icon of an available or incoming vehicle, that vehicle’s status would be updated to indicate it had or would soon have a patient. The mobile emergency system automatically wrote data to the victim’s wristband showing which ambulance would evacuate him. When a first responder read his tag, she got the vehicle ID and then located the ambulance on her handheld.
When an ER opened up in a regional hospital, Henley dragged the icon of an occupied EMT vehicle at the disaster site onto that ER. Instantly, the driver of that vehicle received instructions about where to transport that patient. At the same time, the hospital received information about the vehicle’s estimated time of arrival and the victim’s status.
Peterson was on his cell phone. “We’re overwhelmed here, Governor,” he said. “We need to activate the Volunteer Call System. Thank you, Governor.”
The VCS involved all doctors, nurses and other medical personnel, as well as all available vehicles, drug inventories and almost everything else needed in a disaster. It gave the OEM access to the location of additional people and resources needed to meet the challenge. Peterson ordered that an emergency message go out to all personnel. Once they responded and turned on their tracking devices, they would appear on Henley’s map, and she could direct them to hospitals that required assistance and direct vehicles to secondary pickup points to bring in those less severely injured.
Within 90 minutes, all the victims had been removed from the area. Henley returned to St. Vincent’s to oversee the victims’ treatment. There were more than 100 patients in the emergency room, corridors, medication room, everywhere.
Outside the ER, an elderly woman with a large bandage on her head was lying on a gurney with an IV in her arm.
“Do you have any ID?” an intern asked. The woman motioned toward her pocketbook, which was near her feet. The intern waved a handheld over the bag. “You’ve never been treated here, so I’m going to need your approval to access your medical records.”
The woman nodded. She took the stylus and signed her name in a box on the screen.
“OK, Mary Eckhart, looks like you’re in fine shape. Slight hypertension, arthritic knee, allergic to morphine-based painkillers.”
The woman smiled, but it was clear she was in pain.
“I’ll be right back,” the intern said.
A few minutes later, a loud beeping pierced the noise in the hallway. A nurse had attempted to give Mary Eckhart Percocet, a morphine derivative, and the system sounded the alert because of the patient’s allergy. The intern returned, shouting, “No, no. She’s allergic. We’ll need to give her fentanyl.”
Another nurse ran over to Henley, frantic because she couldn’t find an IV for a man who’d lost a lot of blood. Henley took out her stylus and tapped it a few times. There were no spare units in the building, but several area hospitals were sending equipment. “IV, Priority Urgent,” Henley wrote to the man’s wristband. When IV pumps arrived, the person receiving them would be instructed on who was to get them, in order of priority.
Henley checked the availability of beds. It was clear they’d be filled by the few people who had already been treated. Some patients who needed hospitalization were stable enough to be transported to other medical facilities. Ambulances from around the region were on their way, and she began to assign people transport priorities.
Her cell phone rang.
“Mr. Merriman called,” her husband said. “He can’t locate his wife.”
“Hon, I can’t track her down now. Go to the OEM Web site. Everyone who was treated has a wristband that identifies them. The Web site has some basic information about their condition, and it will say which hospital she’s been brought to.”
“OK, I’ll find her. How are you holding up?”
“OK. We haven’t lost anyone yet. What are the news reports saying?”
“Gas explosion. Thank goodness it wasn’t anything highly toxic.”
Henley hung up and headed to the operating room to see how the surgeons there were managing. She washed her hands near the entrance and donned a surgical gown, cap and booties. A little red light next to the door turned green, indicating that she was properly scrubbed and dressed.
The surgical team was operating on the fifth person from the disaster. A nurse brought the surgeon a fresh tray of instruments. There was a steady beep. One clamp had not been sterilized. The nurse placed it in the autoclave.
“Everything OK, doc?” she asked, clicking on her handheld to check inventories of surgical stents, orthopedic equipment and other critical items. “Anything you need?”
“Lunch break would be nice.”
“Tell me about it. We’re a bit low on A negative blood.” Henley tapped her handheld. “Shipment will be here in 20 minutes—tops.”
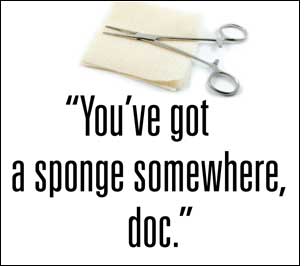
A nurse came over and waved a wand over the patient before the surgeon closed. “You’ve got a sponge somewhere, doc,” the nurse said.
The doctor felt inside the patient and removed a small surgical sponge. “Here we go.”
Henley left the OR and sat on a stool outside to remove her booties. “I thought I’d find you down here.” It was Dr. Gutes, the hospital’s chief administrator. “Nice work, Henley. We saved a lot of lives today.”
“Thank you, sir. The plan and technology we put in place after the Bunding disaster really paid off. This time, we were prepared.”
Photos and illustrations: iStock Photo. Cover photo: René Mansi/iStock Photo
* * *
We’d like to thank the following people for sharing their insight and expertise to help us look into RFID’s future:
• Magda Balazinska, assistant professor, department of computer science and engineering, University of Washington
• Venkat Krishnamurthy, CTO, Checkpoint Systems
• Michael Liard, RFID practice director, ABI Research
• Mike Liebhold, senior researcher, Institute for the Future
• June Ruby, director of manufacturing solutions group, Motorola Enterprise Mobility Solutions
• Alan Sherman, director of marketing, OATSystems
• Chris Warner, senior product manager of RFID, Motorola Enterprise Mobility Solutions
To read more RFID scenarios from the year 2030, click here.